Page Menu
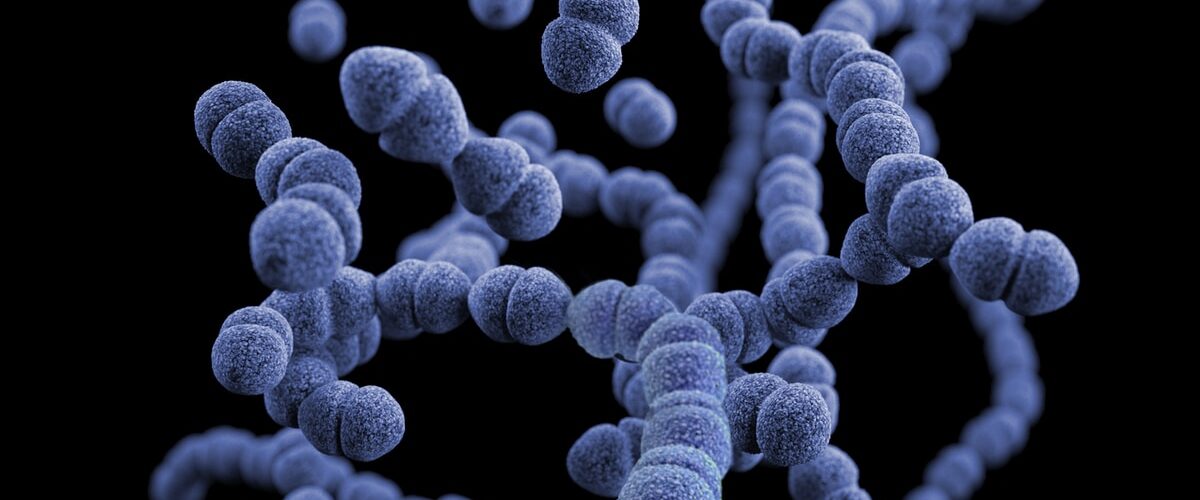
Vancomycin-resistant enterococci (VRE) are a type of bacteria that is resistant to the antibiotic vancomycin. VRE can cause a number of infections in humans, including endocarditis, pneumonia, and meningitis. Some people are more likely to develop VRE infections than others, and factors that increase your risk include having certain medical conditions, being older, and being pregnant.
Key Concepts and Top Takeaways
– Understand symptoms: Watch for fever, chills, and signs of infection like redness or swelling.
– Know the risk factors: Be aware that recent hospital stays and antibiotic use increase vulnerability.
– Practice good hygiene: Wash hands regularly to prevent spreading bacteria.
– Avoid unnecessary antibiotics: Use them only when prescribed to reduce resistance risks.
– Monitor wounds closely: Keep any cuts or surgical sites clean and covered.
– Seek medical attention: Consult a doctor if you suspect an infection or have worsening symptoms.
– Educate yourself on VRE: Learn about vancomycin-resistant enterococcus to better understand it.
– Limit contact with infected individuals: Minimize exposure to prevent transmission.
– Follow treatment plans carefully: Adhere to prescribed medications and recommendations from healthcare providers.
– Stay informed about outbreaks: Keep up with local health advisories regarding VRE cases in your area.
Please Note: This post may contain affiliate links. If you click one of them, we may receive a commission at no extra cost to you. As an Amazon Associate, I earn from qualifying purchases.

Vancomycin is a superb antibiotic that has been used to treat bacterial infections for many years. However, over the last decade or so, strains of bacteria have begun to develop resistance to vancomycin.
Nowadays, vancomycin is only effective against a small number of vancomycin resistant Enterococcus (VRE) strains. This means that if you are infected with a VRE strain, there is a good chance that antibiotics will not work, and you may end up requiring hospitalization or even death.
Fortunately, there are some strategies that can be employed to help prevent infection with VRE strains and thereby protect yourself from these dangerous bacteria. One important step is always to use proper hygiene practices when handling food; this includes avoiding contact with raw meat and poultry, washing hands thoroughly after using the bathroom, and cooking food properly.
Vancomycin resistant enterococcus (VRE) can cause serious complications if not treated. Symptoms of VRE may include diarrhea, fever, and abdominal pain. Some people with VRE may also experience sepsis (an infection that can lead to organ failure).
Complications from VRE can be life-threatening, and treatment may require antibiotics or surgery. There are several risk factors for developing VRE, including health conditions that make you more susceptible to infection, receiving long-term antibiotics, and being pregnant or breastfeeding. The best way to prevent VRE is by being mindful of your surroundings and taking precautions against getting sick. If you develop symptoms of VRE, see your doctor as soon as possible for diagnosis and treatment.
Symptoms of Vancomycin Resistant Enterococcus
Vancomycin resistant enterococci (VRE) are a type of bacteria that are resistant to the antibiotic vancomycin. Symptoms of VRE infection can vary, but may include: a fever, chills, nausea, vomiting, diarrhea, and abdominal pain. In some cases, individuals may also experience blood pressure changes or irregular heart rhythms. If left untreated, VRE can lead to serious health issues such as pneumonia or meningitis.
VRE can be life-threatening. There are several signs and symptoms of VRE infection, and doctors typically use a combination of tests to diagnosis the disease. In some cases, doctors may also treat patients with antibiotics before they have a test to determine if they have VRE.
Vancomycin resistant enterococci (VRE) are bacteria that have developed resistance to the antibiotics vancomycin and teicoplanin. This has made treatment with these antibiotics more difficult, and has led to an increase in the number of cases of fever as a symptom of VRE infection.
Fever can be caused by a variety of factors, but is most commonly the result of an infection or inflammation. When bacterial cells in the body respond to an infection by producing increased amounts of heat, this excess heat can cause symptoms such as fever. In patients with VRE infection, however, fever may also be a sign that their infection is getting worse.
Chills are a common symptom of vancomycin resistant Enterococcus (VRE). VRE is a type of bacteria that can cause serious infections in people, and can be difficult to treat. Symptoms of VRE include fever, chills, and diarrhea. Treatment depends on the severity of the infection and may involve antibiotics or surgery. Chills are one of the most common symptoms of VRE, and can often be a sign that the infection is getting worse. If you experience chills and other symptoms of VRE, talk to your doctor about your symptoms.
Nausea is a common side effect of antibiotics, and it's often one of the first symptoms people notice when their medication doesn't work as intended. Vancomycin-resistant enterococci (VRE) are a type of bacteria that can cause nausea and vomiting, and they're becoming increasingly common in hospitals. VRE infections can be deadly, and if you experience any gastrointestinal problems after being treated with antibiotics, it's important to see your doctor.
Vancomycin resistant enterococcus (VRE) is a type of bacteria that is becoming increasingly more common in hospitals. VRE is responsible for a number of different symptoms, including vomiting. VRE can be difficult to diagnose and often requires multiple tests to confirm the diagnosis. Treatment options for VRE include antibiotics and surgery.
Diarrhea is a common side effect of taking antibiotics, and can be a sign of an infection with Vancomycin Resistant Enterococcus (VRE). VRE is a type of bacteria that is resistant to the antibiotic Vancomycin. When people take Vancomycin, they are creating an environment in their bodies that allows VRE to grow. As a result, people who are infected with VRE often experience diarrhea.
Blood pressure changes as a Symptom of Vancomycin Resistant Enterococcus. Many people may not know that vancomycin resistant enterococci (VRE) is a problem, and when they do, they may be alarmed because the condition can cause blood pressure to change suddenly.
The reason for this is that VRE can form biofilms in the arteries, which can increase the risk of heart attack or stroke. Practicing good hygiene including hand-washing with soap and water is still important even if you have VRE, but it's especially important if you're taking vancomycin because it can make the bacteria more resistant to antibiotics.
Irregular heart rhythms are a common symptom of vancomycin resistant enterococcus (VRE). These infections can cause difficulty breathing, especially in people with asthma or other breathing problems. In some cases, VRE can also lead to heart failure and death.
Vancomycin resistant enterococcus (VRE) is a type of bacteria that is becoming increasingly common in hospitals and other healthcare settings. As of 2016, VRE was found in 18% of isolates from patients in the United States, and it is estimated that the number of cases will increase to 30,000 by 20201. Although most people with VRE develop minor symptoms that resolve within a few days, some people develop serious health problems, including sepsis and meningitis.
Causes of Vancomycin Resistant Enterococcus
Vancomycin resistant Enterococcus (VRE) is a serious bacterial infection that can be fatal if not treated quickly. There are many different causes of VRE, but here are four of the most common: overuse of antibiotics, poor hygiene, hospital acquired infections (HAIs), and genetics.
Vancomycin resistant Enterococcus (VRE) is a serious, life-threatening infection caused by bacteria that has acquired resistance to the antibiotic vancomycin. VRE is most commonly found in patients who are hospitalized or have recently received surgery.
The most common source of VRE infection is healthcare facilities, such as hospitals, nursing homes and hospices. In the United States, VRE infections occur most frequently in people aged 65 years or older and in those with weakened immune systems. There is no vaccine or treatment for VRE infections and they can be fatal if not treated quickly. Scientists are working to develop new antibiotics to treat this infection, but they may not be available for years.
There is no cure for VRE infections, and treatment usually involves antibiotics such as vancomycin. Overuse of antibiotics has led to the development of VRE strains, and it is important to be aware of the risks associated with them so that you can take measures to protect yourself and your loved ones.
Antibiotics are one of the most common causes of vancomycin-resistant Enterococcus (VRE), a bacterial infection that can be life-threatening. VRE occurs when bacteria evolve resistance to antibiotics, which results in less effective treatment. In hospitals, more than half of all cases of VRE are caused by antibiotics.
Antibiotic use in animals and people has led to the development of new strains of VRE that are highly resistant to multiple antibiotics. These strains are difficult to treat and can cause serious health problems in people and animals. Steps need to be taken to reduce the use of antibiotics and prevent the development of resistant bacteria.
Poor hygiene as a cause of vancomycin resistant Enterococcus (VRE) has been well documented. In hospitals, patients commonly share beds, chairs, and other surfaces with others, which increases the risk of cross-infection. Many people also fail to practice good hand-washing habits, which can allow bacteria to spread through contact with open wounds or mucous membranes. VRE is now one of the most common causes of antibiotic resistance in the United States.
Vancomycin resistance is a growing problem in the hospital setting. Hospital acquired infections (HAIs) are a common cause of vancomycin resistant Enterococcus (VRE). In fact, HAIs are now the leading cause of VRE worldwide. VRE can be life-threatening and difficult to treat, so it's important to identify and treat any infections as early as possible.
Research has shown that genetics may play a role in the development of this infection. In studies performed on mice, it was found that VRE strains with certain mutations in their genes are more likely to develop resistance to vancomycin. These mutations occur when the bacteria copies its own DNA incorrectly, which can make it resistant to antibiotics. This suggests that antibiotic treatment may not work as well against these strains and could lead to high mortality rates. However, further studies are needed to confirm these findings.
Risk Factors For Vancomycin Resistant Enterococcus
One of the risk factors for the development of VRE include taking antibiotics improperly or not completing the course of treatment as prescribed. In addition, people who are infected with VRE may also be at an increased risk for other health conditions, such as obesity or diabetes.
Vancomycin resistant enterococcus (VRE) is a growing public health concern as the antibiotic drug vancomycin is no longer effective against this bacterium. VRE can cause serious infections in people with weakened immune systems, and it has been reported in hospitals and nursing homes.
There are several risk factors for developing VRE, including increasing age, having diabetes, cancer or a liver disease, living in a long-term care facility or being immobile. Healthcare providers should be aware of these risks and take steps to prevent infection by VRE, such as screening patients for risk factors and prescribing vancomycin only to those who are seriously ill.
Vancomycin resistant enterococcus is most commonly found in people over 65 years old, but it can also affect people of all ages. Studies have shown that age is a risk factor for VRE. This is because older adults are more likely to have weaker immune systems and be infected with other bacteria that can transform into VRE. In addition, older adults are more likely to have health problems that make them vulnerable to infections, such as diabetes or heart conditions.
Diabetes is a well-known risk factor for developing vancomycin resistance. Diabetics are more likely to develop infections and to take unnecessary antibiotics, which can lead to the development of vancomycin resistance. Additionally, diabetics may have poorer wound healing abilities, which makes them more susceptible to infection and increases their chances of developing VRE-19.
Cancer is a major risk factor for development of vancomycin resistant enterococci (VRE). Previous studies have shown that cancer patients are more likely to develop VRE than individuals without cancer. Furthermore, cancers that metastasize (spread) and those that arise from the skin are particularly dangerous because they can spread the infection to other parts of the body. In fact, about 30% of cases of VRE occur in people with cancer.
There are several ways that cancer can increase your risk for developing VRE. Cancerous cells produce large amounts of vancomycin-resistant bacteria, which can be passed on to others through contact with infected secretions or via the bloodstream. Additionally, cancers often damage healthy tissue around them, which provides an environment in which VRE can flourish.
Liver disease is a common health problem and can increase the risk of developing vancomycin resistant enterococcus (VRE). VRE is a type of bacteria that can cause serious infections in people with weakened immune systems. Liver disease can make people more susceptible to infection by VRE, and can also lead to the development of drug-resistant strains of the bacteria. Treatment with vancomycin or other antibiotics may not be effective against these strains, which could lead to serious health complications.
A recent study published in the journal “PLoS One” has found that individuals with weakened immune systems are at a higher risk of developing vancomycin resistant enterococcus. The study, which was conducted by researchers at the University of California, San Francisco, looked at data from patients who had undergone surgery.
Their findings showed that those with a weakened immune system were 2.5 times more likely to contract vancomycin resistant enterococcus than those without a weakened immune system. This increase in risk could be due to a number of factors, including an impaired ability to fight off disease or damage done to the gut by antibiotics. It is important for hospitals and health care providers to consider this vulnerability when prescribing medications and making decisions about patient care.
Living in a long-term care facility is a risk factor for developing vancomycin resistant enterococci (VRE). A study published in the Journal of Infectious Diseases found that nearly one-third of all VRE infections in long-term care residents were caused by this bacteria. If you are living in a long-term care facility, it is important to take steps to prevent infection, including practicing good hygiene and avoiding coming into contact with people who are sick.
Complications From Vancomycin Resistant Enterococcus
Vancomycin-resistant enterococci (VRE) are a growing problem in hospitals and other healthcare settings. These bacteria can cause serious complications, including bloodstream infections, sepsis, pneumonia, meningitis, and even death. VRE are incredibly difficult to treat, and with increased awareness and vigilance, the number of cases is likely to continue to grow.
Vancomycin resistant Enterococcus (VRE) is a bacterium that can cause bloodstream infections (BSIs). The bacterium is becoming increasingly prevalent, and as vancomycin-resistant strains of VRE become more common, patients are at an increased risk for developing BSI. In fact, the Centers for Disease Control and Prevention (CDC) estimates that there are now more cases of vancomycin-resistant BSI than there are of methicillin-resistant Staphylococcus aureus (MRSA).
BSI is a serious complication that can lead to long-term health problems. Patients with vancomycin-resistant BSI are at an increased risk for death, and they often require intensive treatment in order to improve their condition.
Sepsis is a life-threatening complication caused by infection with a pathogen that has developed resistance to antibiotics. Vancomycin-resistant Enterococcus (VRE) is the most common type of antibiotic-resistant bacteria, and sepsis is the most common serious complication from VRE infection. VRE can cause severe sepsis, which can lead to death in up to 30% of patients.
Sepsis can also occur as a complicating factor in other infections, such as pneumonia, meningitis, and urinary tract infections. The best way to prevent sepsis is to prevent infections in the first place. The Centers for Disease Control and Prevention (CDC) recommends that everyone over the age of 2 years receive routine vaccinations against flu, pneumococcal disease, meningococcal disease, and pertussis (whooping cough).
Pneumonia is a common complication from antibiotic use, and it can be especially dangerous in patients with vancomycin-resistant enterococci (VRE). The Centers for Disease Control and Prevention (CDC) reports that approximately 29,000 people in the United States develop pneumonia each year due to VRE. These infections are particularly difficult to treat, and they can lead to serious health complications, including death.
The best way to avoid pneumonia from VRE is to avoid these bacteria in the first place. The CDC recommends that patients take antibiotics only if they are sure that the infection is caused by a bacterium that is resistant to those drugs. Patients should also contact their doctors if they experience any unusual symptoms after taking antibiotics, such as chest pain or shortness of breath.
Vancomycin resistant enterococcus (VRE) is a bacterium that can cause meningitis in patients who are infected with it. Meningitis is an inflammation of the membranes that cover the brain and spinal cord. The most common cause of meningitis is Streptococcus pneumoniae, but VRE can also cause meningitis.
There are several ways that VRE can cause meningitis. One way is through contact with respiratory secretions from someone who has the infection. Another way is through direct contact with the bacteria itself. In either case, the bacteria can spread from person to person through close contact or by exposure to contaminated objects or surfaces.
Meningitis caused by VRE is serious and can be fatal if not treated quickly.
Treatment for Vancomycin Resistant Enterococcus
Vancomycin resistant enterococcus (VRE) is a serious infection caused by bacteria that are resistant to the antibiotic vancomycin. VRE can spread easily from person to person and can be fatal if not treated quickly. There is no specific treatment for VRE, but the most common approach is to prescribe antibiotics until the infection is resolved. There are various antibiotic options available, but each has its own risks and side effects. The best approach depends on the individual patient's situation and health history.
Vancomycin resistant enterococci, or VRE, are a type of bacteria that can cause a number of infections. There is no one specific treatment for VREs, but often patients will receive antibiotics to try and treat the infection. If the infection is severe, surgery may also be necessary.
VRE is caused by the bacteria Enterococcus faecalis and is usually treated with antibiotics. However, there is now a growing problem with VRE as it becomes resistant to multiple antibiotics. This means that even if a person takes an antibiotic designed to treat VRE, the bacteria may still be able to survive and cause infection. There are several ways that resistance to antibiotics can develop, and scientists are working hard to find new ways to treat this type of bacterial infection.
There is no specific treatment for VRE infections, and current antibiotics are not always effective against this type of bacteria. A recent study found that surgery may be an effective treatment for VRE infections in select patients.
Surgery involves removing infected tissue or organs and can be done in many different ways, including through open surgery or through less invasive procedures such as endoscopy. In the study, which was conducted at a single hospital in the US, 41% of patients who underwent surgery were cured of their VRE infection compared to just 3% of patients who did not receive surgery.
Common Questions About Vancomycin Resistant Enterococcus
What causes vancomycin-resistant enterococcus? Vancomycin-resistant enterococcus (VRE) is a type of bacteria that can resist the effects of vancomycin, a drug used to treat infections. The cause of VRE is not well understood, but it may be caused by the use of antibiotics or other medical procedures. VRE can cause serious infections in people who are infected with it, and it can be difficult to treat. There is currently no cure for VRE, and it is important to be aware of the risk factors for infection and to take steps to prevent these risks if you are susceptible.
Which Enterococcus is resistant to vancomycin? Vancomycin is a powerful antibiotic used to treat a variety of infections. However, it is not always effective against certain types of bacteria. One type of bacteria that vancomycin is less effective against is Enterococcus faecalis. Enterococcus faecalis is one of the most common types of bacteria found in the human gut. This bacterium can cause a range of infections, including urinary tract infections (UTIs), sepsis, and meningitis.
So far, there are three known strains of Enterococcus faecalis that are resistant to vancomycin. These strains have been found in hospitals in Europe and North America. It is important to note that this resistance does not exist in all cases of Enterococcus faecalis infection.
Do patients with VRE need to be isolated? A recent study published in the journal Infection and Immunity suggests that patients with VRE may not need to be isolated. The study was conducted on mice infected with VRE, and it found that while the mice did develop a more severe form of the infection when they were kept isolated, they still recovered. This suggests that, while isolation may be necessary for some patients with VRE, it is not always necessary or beneficial.
How do you overcome vancomycin resistance? There are several ways to overcome vancomycin resistance including: changing the antibiotic selection, using alternative antibiotics when vancomycin is not an appropriate treatment choice, using antimicrobial stewardship programs, and increasing use of oral hygiene measures. Each method has its own benefits and drawbacks, so it is important to carefully consider which approach is best for each individual patient.
Is MRSA resistant to vancomycin? Vancomycin is a drug that is used to treat a variety of infections, including MRSA. MRSA is a type of bacteria that is resistant to many antibiotics, so vancomycin may be less effective against it. However, there is no evidence that MRSA is resistant to all antibiotics and vancomycin may still be effective in treating it. If you are thinking about using vancomycin to treat an infection with MRSA, it is important to discuss the risks and benefits with your doctor.
How common is VRE infection? There is no one answer to this question as it depends on a variety of factors, such as the definition of VRE infection and how it is measured. However, a study published in the journal Emerging Infectious Diseases in 2016 estimated that about 1 in 20 people will develop an invasive VRE infection during their lifetime. This means that there are likely tens of thousands of people in the United States who have contracted VRE and do not know it.
People can become infected with VRE through contact with feces or blood from an infected person. In general, individuals who are most at risk are those who work or live in close contact with people who are infected with VRE. For example, nurses who care for patients who are infected with VRE, doctors and other health professionals who treat these patients, and family members who live with them.
How long can vancomycin-resistant enterococcus survive on surfaces? VRE can survive on surfaces for extended periods of time, making it difficult to control and potentially spreading the infection. Researchers have been investigating strategies to reduce VRE populations on surfaces, but the results are still inconclusive. Some studies have shown that using antimicrobial agents such as chlorhexidine or alcohol can kill VRE bacteria, while others have shown that these methods are not effective in reducing the number of bacteria present. Additional research is needed to determine which method is most effective at reducing VRE populations on surfaces.
What antibiotics treat vancomycin-resistant enterococcus? Vancomycin-resistant enterococcus (VRE) is a type of bacteria that is resistant to vancomycin. There are several antibiotics that can be used to treat VRE infections, but there is no one antibiotic that can be used to treat all VRE infections. Some antibiotics that can be used to treat VRE infections include aminoglycosides (such as gentamicin and amikacin), carbapenems (such as meropenem and ertapenem), and quinolones (such as ciprofloxacin).
How is vancomycin-resistant enterococcus transmitted? Vancomycin-resistant enterococcus (VREC) is a common and lethal form of bacteria that can be spread through contact with respiratory secretions, such as saliva or mucus. While there is no vaccine available to prevent VREC infection, early detection and treatment are critical for those at risk.
VREC can be identified through routine testing of stool samples from patients who are infected or have recently been exposed to the virus. Treatment typically involves antibiotics such as vancomycin. However, VREC has developed resistance to this and other antibiotics, making it increasingly difficult to treat. Prevention of VREC infection starts by avoiding contact with respiratory secretions and keeping your immune system strong by getting vaccinated against influenza each year.
In conclusion, vancomycin resistant enterococcus is a serious infection that can cause a variety of symptoms. It can be deadly in some cases, and it is important to be aware of the risks and symptoms associated with it. There are treatments available, but it is important to seek medical attention as soon as possible if you think you may have contracted the infection.

Kevin Collier is a seasoned health writer at Otchut.com, specializing in over-the-counter medicines, common medical ailments, and general health topics. With a background in healthcare and a passion for making medical information accessible, Kevin aims to empower readers with knowledge to make informed health decisions. When he's not writing, he enjoys researching the latest in health trends and advocating for wellness in his community.