Page Menu
Clostridium difficile is an antibiotic-resistant bacterium that is the primary cause of hospital-acquired “superbug” infections. This infection can lead to severe diarrhea, abdominal pain, fever, and colitis – inflammation in the colon. C. difficile symptoms include diarrhea that may be watery or bloody; fever; loss of appetite; weight loss; tenderness in the lower abdomen; nausea and vomiting. The risk factors for acquiring C.
Key Concepts and Top Takeaways
– Recognize symptoms of Clostridium difficile infection, such as diarrhea.
– Seek medical attention if experiencing severe gastrointestinal issues.
– Maintain good hand hygiene to prevent infection spread.
– Avoid unnecessary antibiotic use to reduce risk.
– Disinfect surfaces regularly, especially in healthcare settings.
– Stay informed about your health history and risk factors.
– Consider probiotics to support gut health after antibiotics.
– Follow a balanced diet rich in fiber to promote digestion.
– Monitor for recurrence of symptoms after treatment.
– Consult a healthcare professional for personalized advice and treatment options.
Please Note: This post may contain affiliate links. If you click one of them, we may receive a commission at no extra cost to you. As an Amazon Associate, I earn from qualifying purchases.

People acquire Clostridium difficile infections by ingesting the spores of the bacterium, which are found in fecal matter. The most common symptom of a Clostridium difficile infection is watery diarrhea. Many other symptoms are also possible. Complications may include extreme cases of diarrhea, intestinal inflammation, colon inflammation, bowel blockages, malfunctions of other organs including the heart and kidney, and death. Symptoms vary depending on the severity of the infection.
Symptoms may present as fever, loss of appetite, abdominal pain, nausea, and sudden weight loss. There is no vaccine for the bacteria, and it is often contracted in hospitals. The bacteria are resistant to many antibiotics and treatment options for C.
Clostridium difficile, also known as “C. Difficile” or simply “C. Diff,” is a bacterium that causes inflammation of the intestines and is most common among people who take antibiotics. It can be passed onto others when someone touches something contaminated with fecal matter and then touches their mouth, eyes, nose, or breaks in their skin.
The overuse of antibiotics, which destroy the natural balance of the gut microbiota, increases a person's risk for contracting this infection. Symptoms include watery diarrhea, fever, loss of appetite, nausea, abdominal pain and/or tenderness. Most cases can be cured with antibiotics, but in some cases, it becomes antibiotic-resistant. The bacterium can live in the environment or on surfaces such as keyboards, door handles, and phone keypads, so it is possible to catch the infection from surfaces outside of hospitals.
Symptoms of Clostridium Difficile
Clostridium Difficile is a bacterium that can cause a number of infections in the intestines. Roughly 80% of cases are hospital based and often occur after a course of antibiotics. Symptoms typically include diarrhea, fever, loss of appetite, nausea, abdominal pain, and flatulence. The most common treatment for these infections includes metronidazole or vancomycin, which kills the bacterium.
This is a nasty bacterium that can invade the gastrointestinal tract and cause severe diarrhea and inflammation of the colon. This bacterium is often spread in hospitals and nursing homes because it has been found in water sources such as sinks and toilets. Hospitals and other healthcare facilities must be diligent in their infection prevention techniques to ensure this bacterium does not spread and put patients at risk.
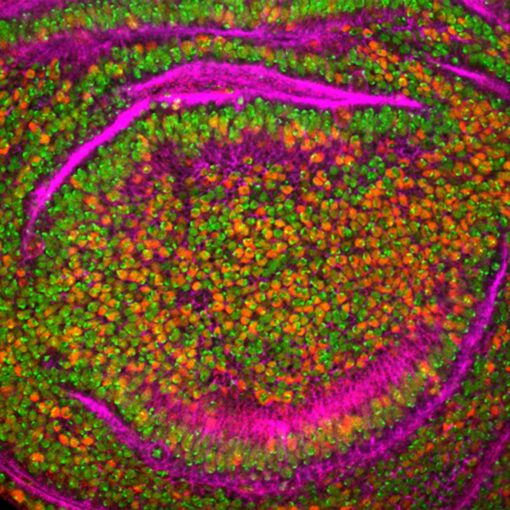
Clostridium difficile, also known as C. diff, is an infection by the bacterium Clostridium difficile. These bacteria produce toxins that can cause stomach pain, diarrhea, or both. The most serious complication of this infection is colitis, inflammation of the colon. The healthy gut contains beneficial bacteria that inhibit the growth of C.diff spores and protect against colonization of other bacteria in the intestine.
Causes of Clostridium Difficile
Clostridium Difficile (C. Diff) is a bacterium that can cause life-threatening diarrhea and colitis in patients. The infection usually occurs after someone takes antibiotics, which kill off the “friendly” bacteria in the digestive tract that usually fight off the C. difficile infection. Some common side effects of C. diff are watery diarrhea, inflammation of the colon, loss of appetite, abdominal pain, nausea, weight loss, fever, etc.
This is a bacterium that can cause diarrhea and colitis, which is inflammation of the colon. The CDC estimates that there are at least 500,000 cases of this infection in the U.S. each year. It is most common in people who have had more than one course of antibiotic treatment, and also among individuals with other serious illnesses such as diabetes and HIV/AIDS.
Clostridium difficile is a bacterium that can cause severe, recurrent diarrhea. It can also cause inflammation of the colon and other parts of the gastrointestinal tract. These symptoms are often caused by taking antibiotics or other medications which reduce the number of beneficial bacteria in the gut. The disease has been on the rise in recent years due to increased use of antibiotics, changes in diet, and an aging population.
Risk Factors for Clostridium Difficile
C. difficile is a bacterium that causes inflammation and ulceration in the colon and can cause diarrhea and colitis. It is more common than it used to be, and new research suggests some of this increase may be linked to some commonly prescribed medications.
Clostridium difficile is a prominent type of bacteria that can cause severe and deadly diarrhea. Diarrhea, caused by Clostridium difficile or C. diff for short, can be spread to other people and can be life-threatening. It has been found to be the most frequent cause of health care-associated diarrheal disease in the United States.
C. difficile, also known as C. diff, is a type of bacteria that lives in the colon. The risk of developing C.diff increases when antibiotics are used to kill bacteria or disrupt their normal functions. Common antibiotic-related causes of C.diff are taking antibiotics for an extended period of time, using antibiotics during pregnancy, being admitted to a hospital, and taking probiotic pills after being on antibiotics too long.
Complications From Clostridium Difficile
Clostridium Difficile, or C. Diff for short, is a bacterium that can cause diarrhea and/or colitis. The CDC estimates that there are about half a million cases of C. Diff annually in the United States alone, with approximately 30,000 deaths each year due to its complications. It has been noted that infants are at the greatest risk due to their underdeveloped immune systems and high ratio of gut bacteria to body mass.
A new and serious complication has been observed in patients with Clostridium Difficile: a sudden and progressive paralysis. This condition often occurs after the patient has had surgery or taken antibiotics, but it is not known what causes the paralysis to happen or how it can be treated. The problem with this complication is that 90% of cases are fatal. It is thought that the paralysis may have an autoimmune component since it happens after taking antibiotics, which are designed to disturb immune responses.
Treatment for Clostridium Difficile
Clostridium difficile is a bacterium that causes diarrhea and colitis in humans. It has become a serious public health problem due to the increase of antibiotic resistance to typical drugs used for its treatment, such as metronidazole and vancomycin. To combat this, physicians have been researching new ways to treat C. difficile, such as fecal transplants.
Clostridium Difficile, which is a bacterium that lives in the gut, can cause serious infection of the digestive system. It is most often diagnosed during or after a course of antibiotics. Symptoms include fever, diarrhea, nausea, and abdominal pain. Patients who get this infection may need treatment with antibiotics and sometimes an enema to get rid of the C-diff spores from their colon.
The rise of Clostridium Difficile has been a major concern for healthcare professionals and patients alike. Traditional methods for treating infectious diarrhea may not always be effective and could lead to complications such as colitis. A new treatment, fecal transplantation, is showing promise in helping those who have recurrent episodes of C. difficile-associated diarrhea. Researchers found that the transplanting of fecal material from healthy donors effectively treated recurring C.
Common Questions About Clostridium Difficile
How can Clostridium difficile be transmitted? The well-studied bacteria Clostridium difficile is a gram-positive spore-forming rod, commonly found in the gastrointestinal tract of humans and rodents. It is also found in soil, where it can remain inactive for long periods of time. When a healthy person ingests C. difficile spores, they can germinate and produce a toxin that will cause diarrhea and abdominal pain lasting up to ten days.
The Clostridium difficile is a bacterial infection that can be transmitted in many ways – including through contact with surfaces or objects, and by contact with people who have the disease. It is also the most common cause of healthcare-associated diarrhea and pseudomembranous colitis, which can pose a significant threat to patients, visitors, and caregivers.
How long is a person contagious with C. diff? C. diff is a bacterium which causes a type of infection known as C. difficile colitis, and it can be very hard to treat. A person is most contagious with C. diff for about two weeks after the first signs of the infection and avoiding contact with people who have been infected can help prevent its spread.
Many people do not know how long they are contagious with C. difficile. This serious infection can cause other intestinal problems such as diarrhea, vomiting, and abdominal pain. Recent studies show that the amount of time someone is contagious depends on the severity of the infection and other factors such as age and health condition. It has been reported that a person could be contagious up to ten days after finishing a course of antibiotics, but it could also be much shorter than this depending on circumstances.
What is the best treatment for Clostridium difficile? Clostridium difficile, also known as C. diff, is a type of bacteria that commonly infects the gut and causes severe diarrhea.
Treatment options for Clostridium difficile include vancomycin, fidaxomicin, or metronidazole. Fidaxomicin is a newer antibiotic with fewer side effects than vancomycin and metronidazole, but it is more expensive and less widely available.
Clostridium difficile, nicknamed “C. Diff” is a type of bacteria that resides in the gut and can be an issue for patients with severely weakened immune systems. Patients that are at risk of the disease are those who have had recent surgery, chemotherapy, or antibiotic treatment. With C. diff being so prevalent in hospitals, it poses a problem for people who are already immunocompromised.
What is the main symptom associated with Clostridium difficile infection? The main symptom associated with Clostridium difficile infection is diarrhea. There are many other conditions that may lead to diarrhea, such as food poisoning or an intestinal virus. To be diagnosed with a C. difficile infection, patients usually will have had diarrhea for at least 14 days and tested positive for toxins in their stool. Treatment options vary and can include antibiotics and digestive enzymes.
Can you get C. diff from a toilet seat? There's a real concern that you can get C. diff from a toilet seat, and if the toilet seat is not clean, then you should avoid using it. The bacteria can be transmitted to surfaces such as the hands, clothes, and even food if they're contaminated by contact with the bacteria. To lessen your chances of getting C. diff, make sure to stay away from dirty surfaces and wash your hands with soap and water afterwards.
When people think about how they can get C. diff infections, they often think that the only way to contract the infection is by eating contaminated food or touching their mouth after handling contaminated surfaces. This is not always the case. As many as 40% of all cases are caused by being in close contact with other people who have C. diff, which means that just being near someone with a C. diff infection can be enough to transmit it to other people.
Should someone with C. diff be quarantined? It's hard to believe that there is even a question about whether someone with C. diff should be quarantined. When you have contracted this infection, it can be life-threatening and will make your immune system very weak. The Centers for Disease Control and Prevention recommends that anyone with C. diff be put into isolation until they are no longer contagious.
Fortunately, there are ways to reduce the chances of contracting this infection, starting with being safe around others.
What foods should be avoided with C. diff? C. diff, also known as C. difficile, is a disease that causes severe diarrhea and other symptoms after a person has been treated with antibiotics. When diagnosed with C. diff, there are many foods to avoid reducing the risk of further complications. One of these foods is milk because it can cause inflammation in the gut which can lead to a worsening condition and diarrhea.
The bacteria Clostridium difficile can cause debilitating diarrhea in individuals. The severity of this disease can lead to dehydration and even death. Furthermore, the bacteria are also responsible for other forms of illness in adults including colitis, cholecystitis, erythromyelitis, proctitis, cystitis, cellulitis, osteomyelitis. When patients are recovering from C.
If you are suffering from C. Diff, you may be wondering what foods to avoid. First, steer clear of any raw foods that might contain harmful bacteria. Likewise, stick to plain breads and pastas so as not to overwhelm your stomach with sugars. Finally, limit how many potatoes you eat because they are heavy on carbs.
Does C. diff affect the brain? C. difficile is a bacterium that causes several forms of contagious diarrhea, and also reduces the effectiveness of antibiotics. Now, there is evidence to suggest that C. difficile may worsen cognitive ability and psychiatric symptoms and lead to irreversible brain damage in patients with underlying psychiatric conditions such as depression or schizophrenia. We know that these patients are at greater risk for becoming infected with C.
In recent years, a new disease known as Clostridium difficile has been rapidly spreading across the world. C. diff affects the intestines and is caused when a person takes antibiotics for an infection. Doctors have been worried about when this strain of bacteria will start affecting the brain because it can lead to serious consequences in terms of cognitive function and even death. So far, there have been no cases of C.
Can C diff be cured with probiotics? A recent article in The New York Times has brought attention to the idea that probiotics may be used to prevent or cure bacterial infections. It was found that when exposed to probiotics, intestinal bacteria populations changed and became more diverse, which made it much less likely for C difficile bacteria to take hold.
Can C diff be cured with probiotics?
The recent coverage of the outbreak caused by contaminated vegetables in Denver has people questioning what they can do to protect themselves. Probiotics are one possible answer, but not everyone is aware of this possibility. Through the use of probiotics, people can help maintain a healthy gut flora, which can be less susceptible to infection with C difficile or other similar bacteria.
In conclusion, the symptoms of Clostridium Difficile are often vague and can easily be mistaken for other illnesses. This infection is caused from a bacterium, which means it can spread from person to person. The risk factors for these bacteria include antibiotic use, hospitalization, and living in a long-term care facility. Complications that may arise from these sinister bacteria can be severe and life-threatening. One example is the inflammation of the colon, which is the disease's most common complication.

Kevin Collier is a seasoned health writer at Otchut.com, specializing in over-the-counter medicines, common medical ailments, and general health topics. With a background in healthcare and a passion for making medical information accessible, Kevin aims to empower readers with knowledge to make informed health decisions. When he's not writing, he enjoys researching the latest in health trends and advocating for wellness in his community.